Categories
Annual Gynecology Screening: What to Do Each Year (and When) for Women’s Health
Nov 06, 2025
What’s next: Below are the steps, intervals, and small checks that keep the whole plan simple and on time.
Your yearly visit: one hour that organizes the next twelve
The annual visit sets baselines and timetables. It includes a history update, blood pressure, weight, counseling (periods, contraception, fertility/menopause), breast and pelvic exam when indicated, and vaccine review. Even if a Pap test isn’t due this year, the visit is still useful: it’s where you book what is due and solve problems early.
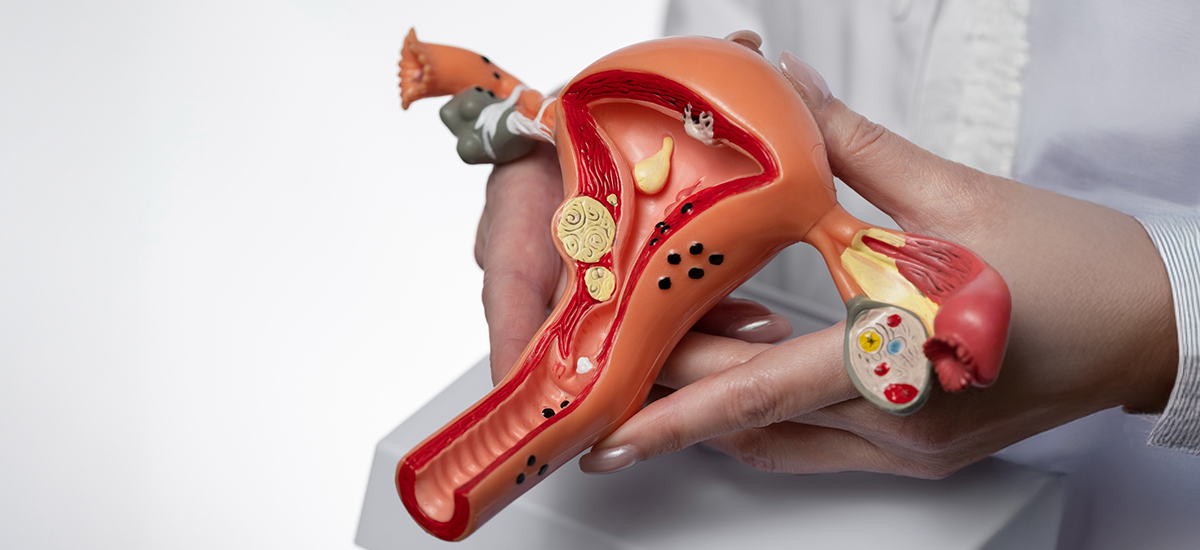
Cervical screening: start at 21, widen options at 30
Cervical cancer screening prevents disease by finding precancer early.
· Ages 21–29: Pap test every 3 years.
·
Ages 30–65 (average risk): one of three choices — primary HPV every 5 years, co-test
(Pap+HPV) every 5 years, or Pap every 3 years. Pick one approach and
stay consistent.
If results are abnormal, your gynecologist
will follow standard pathways so you don’t lose time to worry.
Breast screening: begin at 40, keep a steady cadence
Screen on time and keep going.
· Ages 40–74 (average risk): mammogram every other year. Starting at 40 captures more early cancers and aligns with current national guidance. If you have dense breasts or family history, your gynecologist may individualize timing and modality. Book the next mammogram before you leave the clinic so the rhythm holds.
Sexual health: simple, private, and preventive
Screening is quick and often urine- or swab-based.
· Chlamydia/Gonorrhea: annually if you’re <25 and sexually active; 25+ if you have new or multiple partners or other risk factors.
· Add HIV, hepatitis B/C, and syphilis testing based on history. Results guide treatment and protect future fertility and pregnancy plans.
Bone health and midlife checks: set your future self up well
· DEXA (bone density): start at 65 if average risk; earlier if you have risk factors (long-term steroids, low BMI, prior fracture).
· Your gynecologist also coordinates blood pressure, diabetes, and lipid screening with primary care. The annual visit is where these get scheduled, so nothing slips.
A one-page schedule you can save
Keep this and tick it off at each visit.
| |||||||||||||||||||||||||||||||||||||||||
How to make the visit count (small specifics that add up)
Bring last results (Pap/HPV, mammogram, labs). List medicines and supplements. Note your cycle pattern, pain, mood, sleep, and goals (avoid pregnancy, try to conceive, manage menopause). Ask three direct questions: What am I due for now? What is my plan if a result is abnormal? When is my next check? This keeps the year on rails.
Conclusion:
A consistent annual gynecology screening turns prevention into a habit: one visit to schedule tests on time, update vaccines and contraception, and catch issues early. If you prefer continuity with the best gynecologist for your needs, choose a team that explains intervals clearly, books the next step before you leave, and shares results promptly. BirthRight by Rainbow Hospitals offers structured well-woman visits and coordinated imaging so your plan is set in one sitting.FAQs
1) I felt a new breast lump in the shower. Do I wait until 40 for a mammogram?
No. Book a visit now. Your doctor will examine you and arrange an ultrasound or mammogram based on your age and findings.
2) My periods are suddenly much heavier. Should I wait for my annual check?
Do not wait. Heavy or prolonged bleeding needs a same-week review, blood tests for anemia, and often a pelvic ultrasound.
3) I started a new relationship. Which infection tests should I ask for?
Ask for chlamydia and gonorrhea testing. Add HIV, hepatitis B/C, and syphilis based on your history and your doctor’s advice.
4) I am 22 and sexually active. Do I need a Pap test yet?
Yes. Start cervical screening at 21. From 21–29, a Pap every 3 years is typical if results are normal.