Categories
False Pregnancy (Pseudocyesis): Causes Explained and How Doctors Confirm It
Nov 06, 2025
What’s next: Below are the causes, the verification steps, and the care plan so you can move forward without guesswork.
What “false pregnancy pseudocyesis” means (and how it differs from other terms)
Pseudocyesis is a firm belief of being pregnant with objective signs, yet tests show no pregnancy. It’s different from delusion of pregnancy in psychotic disorders (belief without bodily signs) and different from pregnancy denial (a real pregnancy that the person doesn’t recognise). The working definition sits in psychiatric classification and obstetric texts, and guides how teams talk and test.
Why it happens: the brain–hormone–body loop
There isn’t a single “cause.” Research points to a feedback loop: psychological stressors (infertility, loss, cultural pressure to conceive, relationship strain, perimenopause) interact with the hypothalamic–pituitary–ovarian axis. That stress can alter dopamine and prolactin, and disturb ovulation and periods. The bodily changes (amenorrhea, breast changes, abdominal distension) then confirm the belief and sustain the loop. Some medicines that raise prolactin can add to the picture.
Contexts where clinicians stay alert
Teams see pseudocyesis more often in settings with heavy pressure to conceive, after repeated miscarriages, or when access to early ultrasound is limited. Depression and anxiety frequently travel with it, and need parallel care. Knowing this context keeps the approach compassionate and prevents confrontational conversations that can worsen distress.
How doctors confirm (and what they must rule out)
Verification is structured and quick, because clarity helps symptoms settle.
· Rule out pregnancy: quantitative serum β-hCG and pelvic ultrasound.
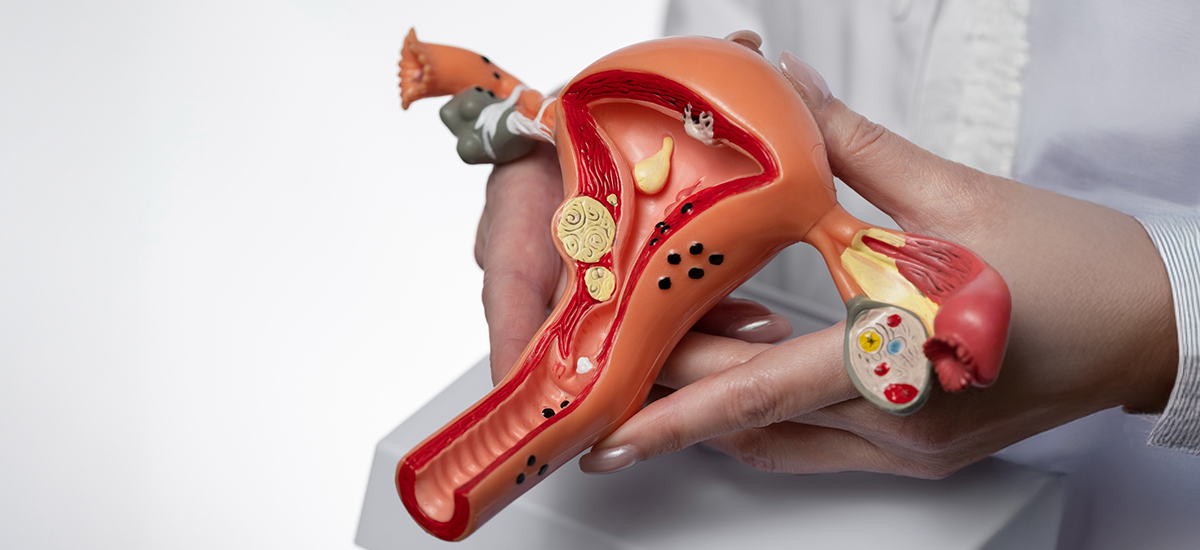
· Check for look-alikes: ovarian cysts, fibroids, abdominal masses, or endocrine issues that mimic pregnancy changes.
· Explain test results carefully: home tests can be misread or rarely false-positive (e.g., recent miscarriage, certain hCG-containing medications). Clear ultrasound images plus a supportive explanation usually break the cycle.
What helps most: a calm plan that treats both mind and hormones
Care works best when it’s joint obstetric–mental health.
· One clear conversation sharing ultrasound and hCG results, with space for grief and questions.
· Psychological support: brief psychotherapy (e.g., CBT or supportive therapy); involve a trusted family member if the patient agrees.
· Treat coexisting conditions: manage depression/anxiety; review drugs that elevate prolactin and adjust if appropriate; address thyroid or other endocrine issues.
· Follow-up timeline: scheduled check-ins prevent rebound symptoms and provide a path if pregnancy is desired later.
Conclusion:
The single idea: pseudocyesis is a real, embodied experience driven by a mind–hormone loop—not “pretending.” Name it, show the tests, and support both psychology and biology. That’s how families move past fear and plan next steps. If you’re searching about false pregnancy pseudocyesis, the specialists at BirthRight by RainbowHospitals coordinate ultrasound, lab testing, and gentle counselling so you have clarity and care in one place.