Categories
Low Estrogen Symptoms: Signs of Low Estrogen Levels You Shouldn’t Ignore
Nov 24, 2025
You hear it all the time—bad sleep, rough mood, someone says it’s hormones and that’s the end of the conversation. That isn’t a plan. The cleaner way is simple. Look for a pattern that matches low estrogen symptoms. Confirm it with focused tests. Treat what’s actually showing up, matched to your stage of life. When you keep it that tight, you stop chasing every ache around the room.
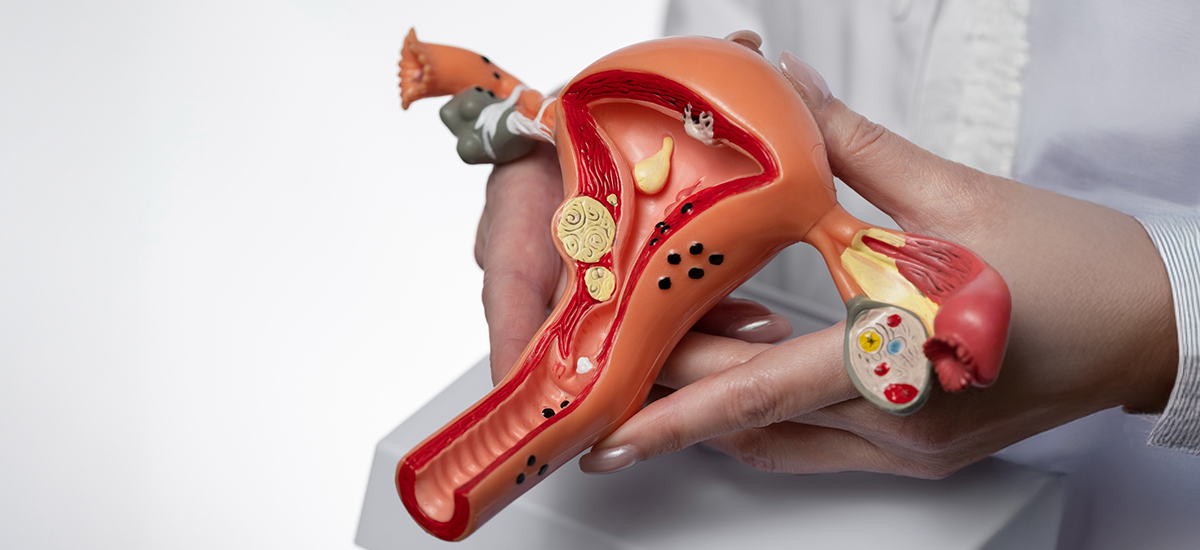
What estrogen does (so the symptoms make sense)
Estrogen keeps periods regular, supports vaginal and urinary tissue, steadies temperature control, helps bones hold calcium, and has a say in sleep, focus, and skin quality. When levels fall, the same systems start to slip: cycles spread out or skip, heat spikes at night, sleep breaks, dryness shows up, and thinking feels duller than it used to. It isn’t mysterious once you lay it out.Who is most likely to run into low estrogen
This shows up in perimenopause, after ovary removal, with ovarian insufficiency, after some cancer treatments, in very low body-fat states or heavy endurance training, and sometimes postpartum with extended breastfeeding. Context matters because it tells you how fast to move and which levers to pull first.The core signs to watch for (use a two-week timeline)
Don’t trust one rough day. Track fourteen days. If three or four of these keep showing up together, pay attention:- Cycles stretching out, skipping, or stopping sooner than expected.
- Hot flashes or night sweats that wake you and don’t quit.
- Sleep falling apart—hard to fall asleep, up too early, or both.
- Vaginal dryness, burning, or pain with sex; slower lubrication.
- Urinary urgency or more frequent UTIs that are new.
- Mood and focus sliding—irritability, lower tolerance, brain fog.
- Drier skin, more scalp hair shedding, small-joint aches.
- Bone clues over time—height loss, easy fractures.
What isn’t specific to low estrogen (so you don’t get sidetracked)
Bloating, weight gain, and fatigue belong to half of medicine; on their own they prove nothing. Low libido has many causes—pain, stress, meds, relationships—so separate those if you want a real fix. Anxiety and depression can sit next to hormone shifts and still need standard care.How to confirm without a fishing expedition
Start with history and exam, then order what answers the question:- Pregnancy test when relevant.
- FSH, LH, estradiol (timing matters; one draw isn’t scripture).
- TSH and prolactin if cycles are off.
- DEXA bone scan if fractures, height loss, or high risk are in the picture.
You don’t need a lab catalog because a video said “hormones.”
Treatment that matches the problem (and actually helps)
Keep it practical and stage-based.- Vaginal symptoms: low-dose vaginal estrogen (tablet, ring, or cream) restores moisture and elasticity; add non-hormonal moisturizers/lubes as needed.
- Hot flashes and broken sleep: systemic menopausal hormone therapy (transdermal estradiol; add progesterone if you have a uterus) is first-line for healthy women near menopause; use SSRIs/SNRIs, gabapentin, or newer NK3-antagonists when hormones aren’t a fit.
- Younger women with cycle gaps/low estrogen states: fix drivers (nutrition, training load, thyroid, prolactin). Consider combined hormonal contraception or cyclic progesterone to stabilize bleeding while the cause is treated.
- After ovary removal or chemo: discuss systemic options or non-hormonal tools promptly; living in a sweat and never sleeping isn’t a plan.
Safety rules that matter
If you have a uterus and use systemic estrogen, you need progesterone to protect the lining. A history of estrogen-dependent cancer, active clotting disease, stroke, or severe liver disease changes the approach. Unexplained vaginal bleeding needs evaluation before or during therapy. Route and dose matter—transdermal often carries a lower clot risk than oral in many patients.When to stop reading and book the visit
Do it now if:- Periods are irregular or absent for 3 months and you’re not pregnant.
- Hot flashes or night sweats break sleep ≥2 nights/week.
- Vaginal dryness or pain interferes with sex or daily comfort.
- Recurrent UTIs with new urgency or leakage.
- Height loss or a low-impact fracture.
Search “gynecologist near me” if you don’t have one; bring notes so the visit counts.